2026 Wound Care Products Explained for Pressure Injury Care
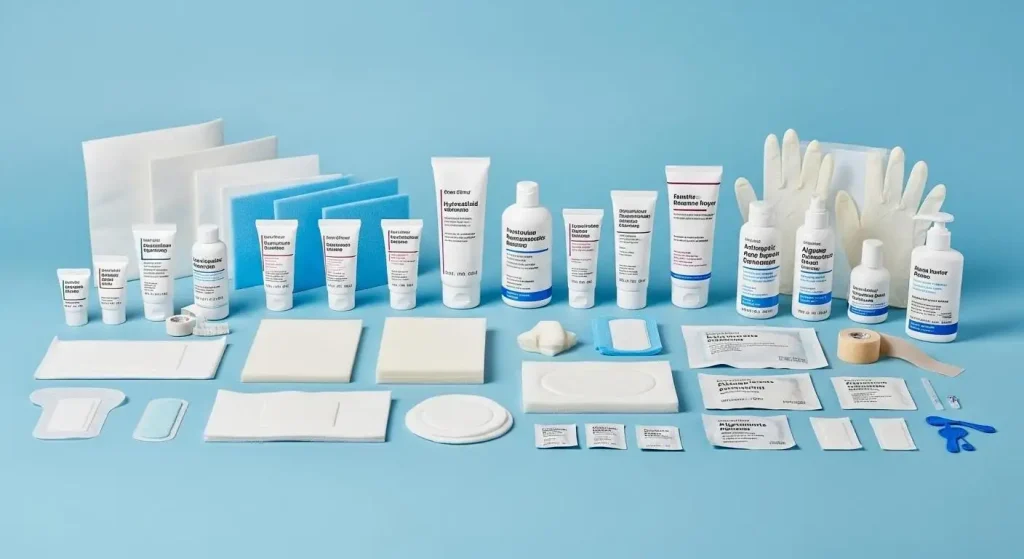
Wound Care Products for pressure injury care can be complex to navigate. This guide will help you master the following: how to choose Wound Care Products by pressure injury stage, how to manage microclimate and exudate, what evidence matters in 2026, and how to build a cost-effective formulary that clinicians will use.

• Match dressing categories to pressure injury stages and exudate levels
• Use prophylactic dressings to reduce hospital-acquired pressure injuries
• Apply advanced Wound Care Products, including NPWT and antimicrobials, appropriately
• Streamline formulary management and staff training to reduce waste and improve patient outcomes.
The following sections translate technical choices into practical actions you can implement today.
The Need for Smarter Wound Care Products in Pressure Injury Care
Pressure injuries remain a high-cost, high-risk issue. In acute care, point prevalence often ranges from 8–9%, while long-term care facilities report 11–28%. Stage III–IV ulcers can cost USD 20,000–150,000 per episode when surgery, prolonged stay, and complications are included. Many cases are preventable when evidence-based bundles are used, yet teams still struggle with microclimate control, shear, device-related injuries, and inconsistent product use.
Pain points include variability in dressing selection, maceration from excess moisture, frequent changes that disrupt tissue, and limited staff time. The right Wound Care Products can reduce dressing changes, improve moisture balance, and protect at-risk sacral and heel areas. Selecting products by wound stage, exudate level, and skin condition is the simplest way to improve consistency and outcomes.
Dressing Categories Explained for Pressure Injuries
Start with a clear map of dressing types and match them to wound needs rather than brand names.
Foam and Silicone-Bordered Dressings
Multi-layer foam with silicone borders is the frontline choice for at-risk skin and shallow Stage I–II pressure injuries. Benefits include microclimate management, shear reduction, and atraumatic removal. Breathable backings allow moisture vapor to escape while the absorbent core locks exudate away to minimize maceration. In prophylactic use on sacrum and heels, multi-layer silicone foam has reduced hospital-acquired pressure injury incidence by 42–70% when applied as part of prevention bundles.
Superabsorbent foam is preferred when exudate is moderate to high, especially around the sacrum where moisture and shear co-exist. Choose contours for heels to offload the Achilles region and avoid adhesive on fragile skin where possible. Limit wear time to manufacturer guidance; change sooner if strike-through occurs.
Hydrocolloid, Alginate, and Hydrogel
• Hydrocolloids: occlusive; promote autolytic debridement; ideal for clean Stage II ulcers with low exudate; avoid in infection or heavy drainage.
• Alginates: calcium alginate/CMC fibers; high absorbency; gel on contact; best for deep cavities and high exudate; add secondary foam.
• Hydrogels: donate moisture; soften eschar and rehydrate dry necrosis; require secondary cover to balance moisture.
• All: secure edges and shield periwound skin with silicone interfaces to reduce trauma at change.
Advanced Wound Care Products: NPWT, Antimicrobials, and Sensors
Deploy NPWT for appropriately selected Stage III–IV pressure injuries - post-debridement and infection control - to accelerate granulation, reduce edema, and manage exudate. Use foam interfaces and guideline pressure ranges, enforce strict offloading, and protect wound edges with drape or silicone to prevent adhesive injury.
Target bioburden confidently with silver or PHMB dressings in critically colonized or high-risk wounds, applied in defined courses with routine reassessment. Avoid unnecessary use in clean Stage I–II injuries.
Leverage 2026 sensor-integrated dressings to time changes precisely, minimizing disruption and preventing strike-through. Adopt where workflows and budgets align.
Put prevention first: microclimate management and offloading drive better outcomes and lower total cost of care. Prophylactic multi-layer silicone foam applied to sacrum and heels at admission has shown substantial risk reduction when combined with repositioning, moisture management, and support surfaces. The mechanism is straightforward: reduced shear at the skin interface, better vapor transmission, and exudate control.
• Apply silicone-bordered foam prophylactically to sacrum and heels for high-risk patients (e.g., Braden ≤ 18)
• Elevate heels fully off the bed with offloading devices; check straps and fit to avoid pressure points
• Manage moisture: use breathable backings and barrier films on fragile periwound skin
• Reposition on a strict schedule; integrate device audits to prevent tubing and mask-related injuries
• Select pressure-redistribution surfaces with adequate immersion and envelopment
Formulary and Procurement: Making Wound Care Products Work
A simplified formulary improves adherence and reduces waste. Group Wound Care Products by clinical function: prophylactic protection, low-exudate occlusive care, high-exudate absorption, moisture donation, antimicrobial control, and advanced therapies. Standardize across units to cut the number of SKUs. Many hospitals achieve 10–20% spend reductions by rationalizing SKUs and see fewer stockouts and product switches. Consolidation also speeds onboarding and reduces documentation errors.
Translate product advantages into operational gains. Atraumatic silicone borders reduce pain and dressing change time. Superabsorbent cores lower the frequency of changes, saving nursing hours. Breathable backings reduce maceration and secondary dermatitis, lowering supply use. Heel-specific shapes improve fit and reduce device-related pressure injuries. Integrate these benefits into clinical protocols and training programs to ensure clinicians understand the rationale for selecting each product option.
Practical Protocols and CTA
Use a simple, repeatable pathway at the bedside:
• Assess risk with a validated scale and inspect sacrum, heels, and device contact points
• Cleanse, debride as indicated, and protect periwound skin with barrier film
• Match dressing to stage and exudate: prophylactic silicone foam for at-risk skin; hydrocolloid for clean, shallow, low-exudate Stage II; alginate plus secondary foam for deep, high-exudate; consider NPWT for Stage III–IV after debridement
• Secure edges, ensure offloading, and document dressing wear time and change criteria
• Reassess every shift; escalate to antimicrobial dressings if bioburden is suspected; refer for surgical consult when needed
Call to Action: To implement an evidence-based 2026 pressure injury care pathway, download our Pressure Injury Dressing Guide, request a sample kit of Wound Care Products for sacral and heel protection, and schedule an in-service with our clinical team. We will audit your current formulary, align categories to your protocols, and help reduce pressure injury incidence while lowering total cost of care.
Submit Your Request
Recent Posts
Tags
- Adult Diapers
- Are custom medical devices safe
- Baby Diapers
- Can respiratory anesthesia be used
- Digital Healthcare
- Do you offer customized consumables
- European Market
- How do you take care of a skin wound
- Industry Trends
- Lady Sanitary Napkins
- Medical Devices
- OEM Medical Devices
- Product Introductions
- Protective Equipment
- Under Pads
- What are custom-made medical devices
- What are diagnostic products
- What are hospital dressing products
- What are medical tube catheters
- What are some common protective equipment
- What are the appropriate applications for hospital dressing products
- What are the appropriate uses for protective equipment
- What is a gynecological examination
- What is a medical consumable
- What is an anesthesia kit
- What is an OEM in medical devices
- what is an wound skin care
- what is can disposable ultrasonic diagnostic
- What is good manufacturing medical devices
- What is hospital-grade protective equipment
- what is medical equipments hospital furniture
- What is medical sterilization wrapping
- What is rehabilitation equipment device
- What medical consumables do you supply
- Where can I find laboratory consumables wholesale
- where can I find medical protection device
- where to buy hypodermic accessories
- where to buy medical apparel
- where to buy medical consumable accessories
- where to find OEM medical device supplier
- where to find rehabilitation equipment supplier









