Burn Treatment Dressings Explain: Moisture Balance and Scar Prevention
Burn Treatment Dressings sit at the point of contact between the injury and recovery. They dictate how quickly a burn closes and how a scar matures over the months that follow. The right plan brings science, practical selection, and a simple timeline together so teams can shorten the open-wound period and cut hypertrophic scar risk without adding unnecessary steps.

This guide focuses on what actually changes outcomes in partial-thickness burns: moisture balance, dressing choice that fits depth and exudate, a staged protocol from Day 0 to closure, and a tight set of metrics to keep care on track. If you manage burns in clinic or on the ward, consider this a blueprint for making Burn Treatment Dressings work harder for patients.
Why Moisture Balance Changes Outcomes
A fresh burn leaks heat and water. If the surface dries, crust forms and keratinocytes can't migrate across the wound bed. Pain rises as nerve endings are exposed, and re-epithelialization slows or stalls. Moisture balance flips that environment. Semi-occlusive Burn Treatment Dressings hold a humid microclimate at the interface while wicking or binding excess exudate. This steadies temperature, reduces trans-epidermal water loss, and shields newly sprouting epithelium from friction.
Two principles matter in daily use. First, a moist wound heals faster than one under dry gauze - this remains consistent across partial-thickness injuries. Second, wear time influences pain and progress. The more you can minimize disturbance, the lower the trauma at change and the more predictable the migration of new epithelium. Many modern dressings support 3 - 7 days between changes when the bed is stable, reducing procedure pain and heat loss.
Breathability is not a guess; it should match the wound's output. A dressing with too little vapor transmission macerates the edges and undermines adhesion. One that breathes too much dehydrates the bed and invites crust. The aim is a moist interface with an MVTR (moisture vapor transmission rate) that supports autolytic debridement but doesn't strip water faster than the wound can replace it. When Burn Treatment Dressings are calibrated to exudate, the bed stays clean, the edges stay intact, and the new epithelium has time to knit.
- The 21-Day Window and Scar Risk
In partial-thickness burns, time to closure is the strongest single predictor of hypertrophic scarring. Full epithelialization within 21 days cuts risk dramatically. Each week beyond that point prolongs inflammation, increases capillary density, and drives collagen to stack vertically. The result is taller, redder scars that remodel poorly and are harder to soften later.
Burn Treatment Dressings that maintain moisture and minimize disruption shorten the open-wound period. Once the surface is closed and dry, silicone therapy helps keep hydration stable and reduces trans-epidermal water loss across the scar. Consistent use - often 8 - 12 weeks - correlates with visible reductions in thickness and erythema. Silicone sheeting or gel is most effective when the epithelium is intact, so bake this into follow-up rather than treating it as an optional add-on. Alignment between closure by Day 21 and early scar care keeps both goals moving together.
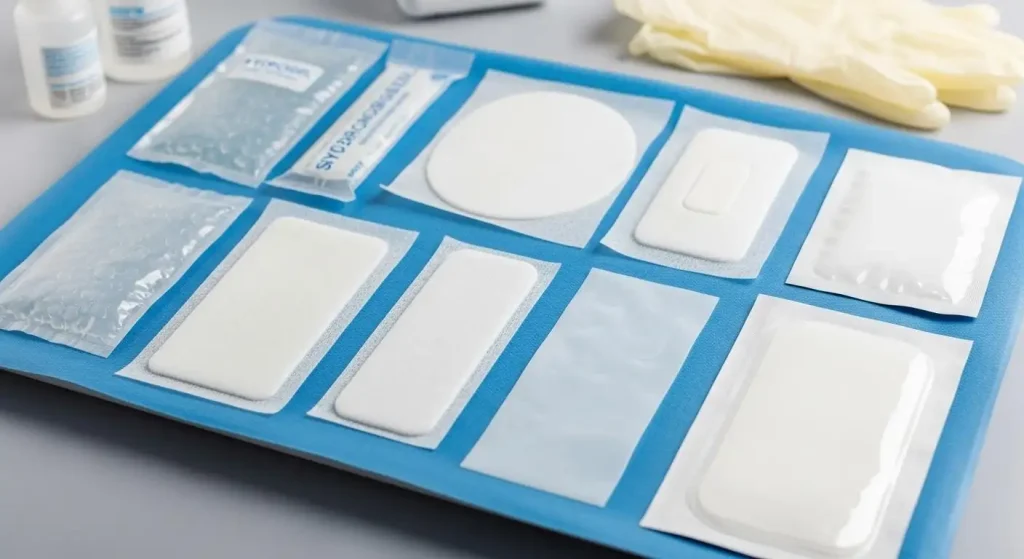
Choosing Burn Treatment Dressings for Real-World Depths
Match the dressing to burn depth, exudate volume, and how you plan to remove it. Favor atraumatic interfaces at every stage and step down as output falls.
•Hydrofiber Or Alginate: High absorption for moderate to heavy exudate. These dressings gel in place, conform to uneven beds, and support autolysis. Useful early when the wound is wet and irregular.
•Silicone Contact Layer Plus Foam: A gentle tack to intact skin with a cushioning, absorbent core. Fits low to moderate exudate and patients prone to pain at changes. The contact layer safeguards fragile new epithelium from shear.
•Hydrocolloid: Semi-occlusive, recommended for low-exudate wounds. Encourages moist autolytic cleansing and longer wear periods. Avoid if critical colonization or infection is suspected.
•Film Dressing: Vapor-permeable barrier for superficial burns and donor sites. Very low absorption, strong protection against friction and contamination. Best used once exudate is minimal.
•Silver-Releasing Options: Consider for rising bioburden or likely critical colonization, particularly as bacterial counts near the ~100,000 CFU/g threshold. Pair with reassessment of wear time and documented clinical response.
Non-Adherent Layers: Place as a secondary, low-tack interface to prevent adherence. Avoid dry gauze on viable tissue; it binds to the bed and tears epithelium on removal.
Across all categories, tune MVTR to the wound. This helps prevent edge whitening and bogginess, cuts strike-through, and reduces unplanned changes. When conditions stabilize, aim for longer wear to protect temperature and allow uninterrupted epithelial migration. Burn Treatment Dressings that hold a steady microclimate are the ones that consistently shorten the open period.
A Practical Protocol From Day 0 to Closure
Clear steps limit variability and keep the team focused on the 21-day target.
- Day 0 - 3: Set the Trajectory
•Cleanse with non-cytotoxic solutions; remove debris without injuring viable tissue.
•Debride loose necrotic slough when clinically appropriate to decrease bioburden and present a receptive wound bed.
•Select a primary Burn Treatment Dressing that maintains moist healing and suits the anticipated exudate; secure with a breathable overlay to help regulate temperature.
•Limit manipulation. Preserve new epithelium from shear and use atraumatic, low-tack removal methods.
- Days 4 - 10: Control Moisture, Reduce Trauma
•As exudate eases, move to a thinner foam or film to avoid maceration and keep edges seated.
•Inspect the periwound for whitening, bogginess, or breakdown at the margins; adjust MVTR if needed.
•Watch bioburden indicators: new odor, a sudden exudate surge, delayed granulation, or increased pain. Consider a silver-releasing dressing and shorten wear intervals while reassessing the wound bed.
•Keep removal gentle. A silicone contact layer can lower pain and preserve fragile epithelium.
- Days 11 - 21: Close Without Interruptions
•When >90% epithelialized, transition to low-adherence coverings that shield from friction without drying the surface.
•Keep changes to a minimum. Less manipulation reduces setbacks.
•If complete closure seems improbable by Day 21, transition to grafting or advanced therapies. A decisive step at three weeks often prevents months of hypertrophic scarring.
- What to Monitor
•Time To 100% Epithelialization: Target 21 days or fewer for partial-thickness burns.
•Wear Time And Changes Per Week: Aim for two to three changes or fewer when stable.
•Periwound Integrity: No maceration; minimal edge trauma; stable, consistent margins.
•Pain Scores At Change: Seek continuous decline; modify interfaces if pain rises.
•Bioburden Signals: Odor, exudate spikes, color change, or stalled granulation should trigger review.
Product Spotlight and Call to Action
Our integrated Burn Treatment Dressings system integrates a soft silicone contact layer, a high-capacity gelling core, and a breathable, waterproof film. An optional silver component adds targeted bioburden control for at-risk wounds. The design turns clinical priorities - moisture balance, atraumatic changes, and longer wear - into practical gains for patients and teams.
•Less Pain At Change: The silicone interface adheres to intact skin rather than the wound bed, protecting new epithelium and lowering change-related pain.
•Moisture On Demand: The gelling core locks exudate vertically, limiting lateral spread and periwound maceration for steadier healing.
•Fewer Interventions: Typical wear times of 3 - 7 days reduce changes, clinic visits, and heat loss, enabling uninterrupted epithelial migration.
•Targeted Bioburden Management: Sustained ion release from the silver option addresses local bacterial pressure without frequent topical rotations.
•Conformable Protection: Thin, flexible profiles wrap hands, joints, and facial contours, reducing edge lift and shear on mobile sites.
Standardize moisture balance and scar prevention across your pathway. Adopt Burn Treatment Dressings that align with the 21-day closure goal and pair closure with a silicone-based scar regimen. Contact our clinical team for samples, protocol templates, and training. Bring a proven Burn Treatment Dressings system into your practice and deliver faster closure with lower scar risk.
Submit Your Request
Recent Posts
Tags
- Adult Diapers
- Are custom medical devices safe
- Baby Diapers
- Can respiratory anesthesia be used
- Digital Healthcare
- Do you offer customized consumables
- European Market
- How do you take care of a skin wound
- Industry Trends
- Lady Sanitary Napkins
- Medical Devices
- OEM Medical Devices
- Product Introductions
- Protective Equipment
- Under Pads
- What are custom-made medical devices
- What are diagnostic products
- What are hospital dressing products
- What are medical tube catheters
- What are some common protective equipment
- What are the appropriate applications for hospital dressing products
- What are the appropriate uses for protective equipment
- What is a gynecological examination
- What is a medical consumable
- What is an anesthesia kit
- What is an OEM in medical devices
- what is an wound skin care
- what is can disposable ultrasonic diagnostic
- What is good manufacturing medical devices
- What is hospital-grade protective equipment
- what is medical equipments hospital furniture
- What is medical sterilization wrapping
- What is rehabilitation equipment device
- What medical consumables do you supply
- Where can I find laboratory consumables wholesale
- where can I find medical protection device
- where to buy hypodermic accessories
- where to buy medical apparel
- where to buy medical consumable accessories
- where to find OEM medical device supplier
- where to find rehabilitation equipment supplier









